- Conditions
- Pulmonary embolism
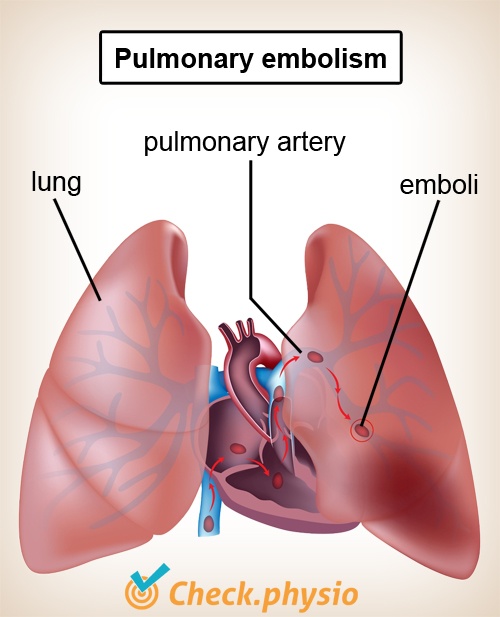
Pulmonary embolism Blockage of a pulmonary artery /PE
Introduction
A pulmonary embolism is a blockage of a pulmonary artery, usually caused by a blood clot. This has negative effects on the oxygen uptake in the lung and causes shortness of breath.
As the symptoms can vary significantly in severity, the diagnosis is often missed.
Description of the condition
An embolism is a blockage of a vein or artery. Usually this is caused by a blood clot formed at one location that blocks a blood vessel at another location. In addition, the blockage can - in exceptional cases - be caused by an air bubble (when piercing a blood vessel), or by other forms of blockage.
In the case of a pulmonary embolism, the blockage is located in the pulmonary arteries. These are the blood vessels that carry deoxygenated blood around the lung to supply the blood with oxygen. As the pulmonary artery branches into smaller blood vessels, the risk of the embolism blocking the blood vessel increases.
The blockage reduces the flow of blood behind the blockage. Parts of the lung behind the blockage are skipped. Therefore, the blood is supplied with oxygen less effectively in the lung. This results in a decreased oxygen concentration in the blood. In medical terms, we call this a decrease in the 'oxygen saturation' of the blood.
Cause and origin
A pulmonary embolism usually occurs when a blood clot forms in one of the large veins in the thigh or pelvis (thrombosis). This clot can dislodge and enter the lungs via the circulation.
Risk factors for developing a pulmonary embolism include:
- Lack of exercise.
- Obesity (severe excess weight).
- Cancer.
- Major surgery (particularly in the abdomen).
- Pregnancy.
- Severe asthma.
Signs & symptoms
The symptoms can vary significantly in severity. Possible symptoms include:
- Shortness of breath, feeling of tightness.
- Increased breathing rate.
- Pain on the chest (becomes worse when breathing).
- Sudden need to cough.
- Increased heart rate.
- Coughing up blood.
- Blue discolouration of the lips and/or fingers.
- Loss of consciousness.
If the blood clot is very large, it can block the access to the lungs in a fatal manner. However, this is very rare.
Diagnosis
The doctor will estimate the symptoms and assess whether these may be caused by a pulmonary embolism.
If there is a relatively high risk of pulmonary embolism, the patient will be referred for a CT scan. Contrast fluid will be injected into the circulation, making the pulmonary arteries and their branches visible. If all the branches are clearly visible, then a pulmonary embolism can be ruled out.
If the risk of a pulmonary embolism is deemed low, then a blood test will first be performed. Based on the result of this blood test, the decision can be made to perform a CT scan after all.
Treatment and recovery
The patient will receive anticoagulants to prevent expansion of the existing clots and to combat the formation of new clots. Thrombolysis can be performed in severe cases. This involves the use of powerful drugs to dissolve the clot.
More info
You can check your symptoms using the online physiotherapy check or make an appointment with a physiotherapy practice in your area.
References
Zaagman-van Buuren, M.J. & Jong, J.T.E. de (1997) Algemene ziekteleer Tweede, herziene druk. Houten/Diegen: Bohn Stafleu van Loghum.
Walen, S., Kuipers, A.F., Berg, J.W.K. van den & Damoiseaux, R.A.M.J. (2011) Longembolieën Huisarts & Wetenschap: 54(3) 166-169.
